Endoscopy in Westchester, NY – Upper Endoscopy Services
At Gastroenterology of Westchester, we provide expert endoscopy procedures in our Yonkers office to help diagnose and treat upper gastrointestinal conditions. If your doctor has recommended an upper endoscopy (EGD), rest assured you’re in experienced hands.
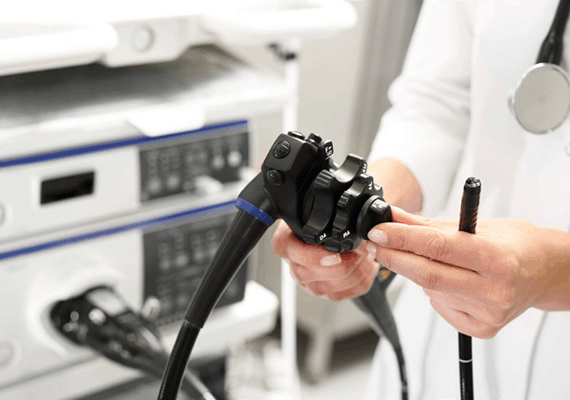
What Is an Upper Endoscopy?
An upper endoscopy, also known as an esophagogastroduodenoscopy (EGD), is a diagnostic procedure used to examine the esophagus, stomach, and duodenum (the upper part of the small intestine). During this quick outpatient procedure, a flexible tube with a camera (endoscope) is gently inserted through the mouth to provide a detailed view of the upper digestive tract.
Upper endoscopy is essential for detecting issues like:
- Gastroesophageal reflux disease (GERD)
- Ulcers
- Inflammation
- Swallowing difficulties
- Abnormal growths
- Precancerous changes or cancer
Why Might You Need an Endoscopy?
A doctor may recommend an upper endoscopy to investigate symptoms such as:
- Persistent abdominal pain or nausea
- Frequent heartburn
- Vomiting or gastrointestinal bleeding
- Trouble swallowing
This procedure is more accurate than X-rays in diagnosing upper GI problems and allows your gastroenterologist to take biopsies or perform minor treatments during the same visit.
Preparing for an Upper Endoscopy in Westchester
We’ll provide specific instructions during your consultation, but general prep usually includes:
- Fasting for 8 hours before your procedure
- Stopping certain medications (especially blood thinners)
- Informing us of any medical conditions, allergies, or supplements you’re taking
Compared to colonoscopies, upper endoscopy prep is simple – just fasting. No laxatives or full-day preparation required.